
What you eat and how you eat can have a major impact on digestive problems.
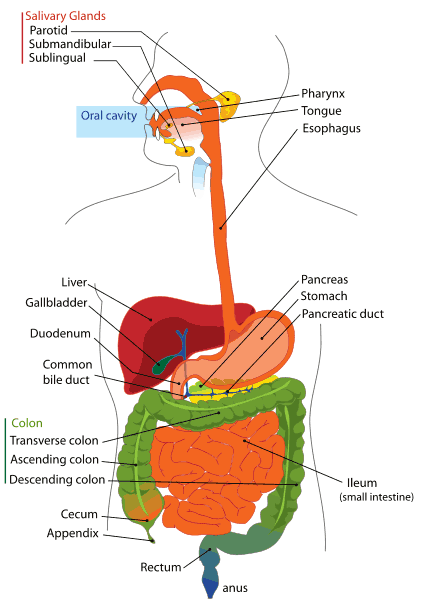
The digestive system is made up of the digestive tract, the salivary glands, liver, gall bladder, and pancreas. The digestive tract is essentially a long tube. In total, it is about 7.3m long and composed of a series of joined sections made up of the mouth, oesophagus, stomach, small and large intestines, rectum, and anus.
tract, the salivary glands, liver, gall bladder, and pancreas. The digestive tract is essentially a long tube. In total, it is about 7.3m long and composed of a series of joined sections made up of the mouth, oesophagus, stomach, small and large intestines, rectum, and anus.
How it works?
The role of the digetive tract is to break down food and transport nutrients throughout the body for energy, growth, and repair. It is also responsible for eliminating waste from the body. The rhythmic contraction of the muscles lining the oesophagus is called peristalsis. This action moves food into the stomach and prevents any stomach contents from going backwards into the oesophagus (reflux). To aid in this function there is a ring of muscles at the bottom of the oesophagus called the lower oesophagi sphincter. Medical problems occur when there is a structural or functional change along the digestive tract or in the associated organs.
What can go wrong?
Disorders of the digestive system that can in some way be relieved, treated, or prevented by dietary or lifestyle. The most common digestive disorders are usually short term problems and include indigestion, diarrhoea, and constipation. A common cause of indigestion is gastro-oesophageal reflux disease (GORD), in which acidic stomach juices are regurgitated. Peptic ulcer, which affect either the stomach or the duodenum (the first part of the small intestine) may persist or recur. Some disorders, for example Crohn's disease and ulcerative colitis, cause inflammation of the intestine and affect the absorption of nutrients. Other disorders, such as lactose intolerance and coeliac disease, are a result of a reaction to a substance that is present in food. The dietary and lifestyle changes you can meke to combat these disorders, and treat any side effects.
What are digestive disorders?
Diarrhoea, constipation, and indigestion are common, and there are measures you can take to prevent and treat them. However, diarrhoea may be a symptom of an infection or a long term problem, such as irritable bowel syndrome (IBS) or an inflammatory bowel disorder such as ulcerative colitis or Crohn's disease. If diarrhoema persists, see your doctor. Gastro oesophageal reflux (GORD) is a common disorder of the oesophagus and a cause of indigestion. Attacks can be mild, but may leave your oesophagus scarred. Peptic ulcer is commonly due to a bacterium called Helicobacter pylori. Many digestive disorders can be successfully managed by following your doctor's advice and making lifestyle changes.
What are the risk factors for digestive disorders?
Some of the known risks for digestive disorders are outlined below, these include diet and lifestyle, age, gender and family history.
Diet and lifestyle
A diet that does not include a sufficient amount of fiber may lead to some digestive disease. For example, diverticular disease is more common in the West, where intake of fibre tends to be low because of the popularity of refined grain products. Anyone who is overweight or has a high fat diet is at risk of developing gall stones. Drinking alcohol, smoking cigarettes, and emotional stress may all trigger or aggravate existing stomach ulcers ir interfere with their healing.
Age
As people grow older, the motility of their intestinal tract decreases, and therefore food and waste move through the intestine at a slower rate, which increases the risk of constipation. Similarly, diverticular disease is more common in people over the age of 50, and over half of the age of 70 and nearly everyone over 80 has this disorder. About ten per cent of people in US suffer from irritable bowel syndrome (IBS), a condition that is most common in those aged 15-40 years. Similarly, Crohne's disease and ulcerative colitis most commonly first develop in young people aged 15-30 years.
Gender
Some gastrointestinal disease, such as peptic ulcer, do occur more commonly in men than in women. But gall stones and IBS are more common in women than in men.
Family history
Some digestive disorders, such as coeliac disease, are genetic and can run in families. Family members of people who have been diagnosed with a genetic digestive disorder may be offered tests to see if they are at risk of developing the disorder. Between 15 and 30 per cent of people with Crohne's disease and ulcerative colitis have a family history of these conditions, suggesting that genetics are involved in their development too.
Nutrition for digestive disorders
Nutrition plays a big role in many digestive disorders because what you eat has an important effect on your gastrointestinal (GI) tract. If your GI tract is abnormal in any way your doctor will suggest specific dietary changes to help alleviate some of your symptoms. Some of this dietary changes may help correct and prevent the problem. For example: increasing the amount of fibre in your diet and drinking more water will help prevent constipation; and excluding gluten, a specific type of protein, may be required for the rest of your life if you have coeliac disease. Although this may sound difficult, it could save your life and you will be grateful to be able to enjoy your meals again without suffering from painful symptoms afterwards. Your doctor may advice you to change your lifestyle. For example, if you have reflux disease you should avoid lying down after eating; and if you have a peptic ulcer you may need to limit foods and drinks containing caffeine.
Making the appropriate changes to manage your digestive disorders requires patience and a trail and error period. You may find it helps to write down the offending foods that give you wind or cause you to feel bloated. If this continues to happen over and over again, than eliminating these foods may be beneficial to you. But remember, if you eliminate food groups from your diet you may need to take supplements. For example, those who avoid dairy products will need a calcium supplements to prevent osteoporosis from developing. A lot has changed over the years with regards to nutrition for digestive disorders.
Treating constipation
A diet that is high in animal fats, such as meat, cheese, and eggs, and refined sugar, but low in fibre from vegetables, fruits, and whole grains is a common cause of constipation. The infrequent and difficult passage of stools is particularly common on older people. This is because gut motility decreases with age, resulting in food and waste taking them regularly. It is far more effective to treat constipation through changes to your diet. In addition, regular exercise will help stimulate intestinal activity and improve the motility of the intestinal tract.
Increase your fluid intake
If you suffer from constipation, increase your fluid intake. Aim to drink about 2 liters of water a day. Dry stools are more difficult and painful to pass, but drinks add bulk and fluid to the stool, making it easier to expel. Limit alcohol and caffeine because they can lead to dehydration, creating stools that are hard and more difficult to pass.
Increase your fibre intake
Dietary fibre in food traps water and adds bulk to the stool, making it move through the gut more quickly.
- Make sure that you eat lots of fresh fruits and vegetables. Include foods with a natural laxative effect, such as prunes or prune juice, apricots and apples.
- Avoid eating processed or highly refined foods, which are high in sugar and carbohydrates and low in fibre.
- Increase your fibre intake by eating more whole grains, wholemeal bread and pasta, vegetables, fruits, and pulses. Aim to eat five servings of grans and grain products daily.
- Switch from white bread, pasta, and rice to wholemeal of whole-grain types.
- Eat a high fibre breakfast cereal. Bran cereals are particularly high in fibre and can be livened up with toppings, such as aliced banana, raisins, or strawberries.
Treating diarrhoea
Diarrhoea - the frequent passage of loose, watery stools is often caused by infections from contaminated food of water.
How to prevent diarrhoea?
Good hygiene and awareness of the sources of food contamination will help you to avoid diarrhoea.
- Wash your hands after using the toilet and changing baby's nappies.
- When travelling overseas, drink only bottled water, carbonated soft drinks and drinks made with boiled water such as tea and coffee. Do not drink tap water or have ice that has been made from tap water.
- Peal fruits and vegetables.
- Frequently wash bathroom and food preparation surfaces.
- Avoid meat or fish that is raw or rare, or that is not served hot.
The following suggestions will help easy your symptoms.
- Avoid very hot or very cold liquids, coffee, alcohol, or coffined soft drinks, all of which can irritate the intestine.
- If you can tolerate food, eat yogurt with live cultures (to replace gut flora) and avoid insoluble fibre (whole grains) until the diarrhoea has resolved.
- Eat bland, non fatty foods, that are easily digested, and avoid milk, red meats, and highly seasoned food.
- Replace lost fluid and electrolytes (minerals dissolved in fluids) with water, fruit juices diluted with water, re hydration drinks. Try to drink at least 500ml of fluid every one to two hours to prevent dehydration.
- Read product labels and check with your chemist if medications and diet products contain sorbitol or lactulose, both of which can cause diarrhoea, discontinue taking them if possible.
- If the bout of diarrhoea is a short term problem, avoid high fibre foods, such as whole grains and fresh vegetables and fruits, all of which can be difficult for the irritated intestine to digest. If the diarrhoea last for more than two weeks, increasing soluble fibre intake may help, but you should aee your doctor.
Treat indigestion
How to relieve mild attacks of indigestion pain or discomfort in the stomach or upper abdomen that usually comes on after eating a meal. The complain may be accompanied by nausea, belching, and bloating. It is caused by eating or drinking too much or by stress, or may be a symptom of an underlying disorder such as a peptic ulcer.
- Eat small, low fat meals and snacks, such as fruits, pretzels, crispbreads, and low fat yogurt frequently, and at regular times during the day.
- Have drinks between meals, rather than with meals.
- Avoid foods that may irritated the stomach, such as caffeine, spearmint, peppermint, citrus fruits, spicy foods, high fat foods, and tomato products
- Take a walk after meals, but do not do any strenuous exercise for at least one hour after eating.
- Some people find that a cup of herbal tea, such as peppermint, fennel, or chamomile, provides relief.
- Always eat slowly and chew your food thoroughly.
- Avoid lying down for at least two hours after eating a meal.
- If you smoke, you should try to stop, since smoking may worsen the symptoms.
- Try having a warm milk before bed, and use extra pillows to raise your head.
- Do not take aspirin or ibuprofen for pain relief since these medications can irritate the stomach.
- If stress might be a cause of your indigestion, try to include relaxation techniques in your life, such as yoga or meditation worsen the symptoms.
- Try an antacid medication, which can relieve the symptoms of indigestion by neutralizing stomach acid.
- If you are overweight, which may worsen symptoms, try to lose weight.
- See your doctor if your symptoms become worse or do not improve after two weeks or if your indigestion recure.
Treating gastro-oesophageal reflux (GORD)
GORD is common cause of indigestion that occurs when acidic stomach juices are regurgitated into the oesophagus (the tube from the throat to the stomach). These stomach juices irritate the oesophagus, causing inflammation and pain (heartburn), and this can cause permanent scarring if the condition persists. The main cause of GORD are poor tone in the ring of muscle at the end of the oesophagus (the lower oesophageal sphincter) and increased abdominal pressure bue to obesity or pregnancy. It is important to follow a low fat diet since high fat meals tend to decrease sphincter pressure, slowing the movement of food to the stomach and exposing the oesophagus to irritants. Other key ways to treat GORD include losing weight if you are overweight and avoiding fatty foods, alcohol, chocolate, and coffee as much as possible.
throat to the stomach). These stomach juices irritate the oesophagus, causing inflammation and pain (heartburn), and this can cause permanent scarring if the condition persists. The main cause of GORD are poor tone in the ring of muscle at the end of the oesophagus (the lower oesophageal sphincter) and increased abdominal pressure bue to obesity or pregnancy. It is important to follow a low fat diet since high fat meals tend to decrease sphincter pressure, slowing the movement of food to the stomach and exposing the oesophagus to irritants. Other key ways to treat GORD include losing weight if you are overweight and avoiding fatty foods, alcohol, chocolate, and coffee as much as possible.
Read more about heartburn (often called acid indigestion).
Treating irritable bowel syndrome
People with irritable bowel syndrome (IBS) the colon (the major section of the large intestine) is abnormally sensitive to stimuli such as excess wind, stress, high fat or fibre rich foods, caffeine, and alcohol. These stimuli can irritate the colon and cause pain, cramps, and diarrhoea. Women with IBS may have more symptoms during menstrual periods, suggesting that reproductive hormones can aggravate the condition. Many people state that the symptoms occur after they eat or when they are under stress.
A balanced diet can help alleviate IBS symptoms. You may find it helpful to keep a food dairy to identity which foods cause the the most discomfort and try to eliminate these from your diet. The foods may be different for each person, for example, some people find onions and mushrooms cause wind, bloating, and discomfort, while others find relief from omitting wheat.
Even if you find that most dairy products are difficult to tolerate, do not rule out yogurt. Yogurt may be better tolerated because it contains organisms that supply lactase, the enzyme needed to digest lactose (the sugar in milk). Lactose free milk is also option. Since dairy products are an important source of calcium, consider drinks enriched with calcium or take a calcium supplement if your body cannot tolerate dairy products.
High fibre foods, such as wholemeal bread, whole-grain cereal, pulses, fruits, and vegetables, help to avoid intestinal cramps and spasms, and constipation, although if you suffer from diarrhoea, a low fibre diet is better. It is also best to avoid coffined drinks such as tea, coffee, and cola, which stimulate the colon. Many find herbal teas, especially peppermint and fennel, soothing. Fruit juice contains a lot of fructose, which can aggravate symptoms of IBS and contribute to diarrhoea. It is best to sick to drinking mineral water to help flush out your system. In addition, smoking can exacerbate the symptoms of IBS, so it is important to quit if you smoke.
Treating and preventing peptic ulcer
The goals of nutritional treatment for peptic ulcer - damage to the stomach lining (stomach ulcer) or the first part of the small intestine (duodenal ulcer) are to reduce and neutralize stomach acid and to maintain the stomach lining's resistance to the acid. Reducing stomach and helps alleviate symptoms and allows sores to heat.
There is not specific diet for ulcer, each person must discover which foods cause discomfort and avoid them. You may find the following tips helpful:
- Avoid bedtime snacks, since symptoms often occur in the night.
- Eat three meals daily, avoid skipping meals, and limit your intake of spicy, fatty, or other foods, that cause discomfort
- Limit your alcohol intake and avoid drinking on an empty stomach
- Limit caffeine intake by reducing your intake of coffee, tea, cola, and chocolate
- Avoid smoking and passive smoking as smoke may increase the secretion of stomach acid, increase the frequency of duodenal ulcer, and delay healing.
Peptic ulcer are commonly associated with Helicobacter pylori infection. The infection is thought to be spread by unsanitary living conditions. It infects the stomach and releases substances that reduce the effectiveness of the layer of mucus that protects the stomach lining from its own acidic juices. The acidic juices then erode the lining of the stomach or the duodenum, allowing a peptic ulcer to develop. A combination of antibiotics and ulcer healing drugs will usually clear up the ulcer.
Preventing and treating gall stones
Gall stones are formed from bile, a cholesterol rich liquid made by the liver and stored in the gall bladder that aids the digestive process. Gall stones are more common on women, in people over the age 40, and those who are overweight and eat a high fat diet. A family history of gall stones is a risk factor.
Low-fat, high-fibre diet
Avoiding fatty foods and increasing your consumption of fibre by eating more high fibre foods such as bran, soya, guar gum, and pectin, which is found in many fruits and vegetables, can help prevent gall stones and relieve the discomfort caused by existing stones. Regular exercise may also decrease the risk of developing gall stones. If you are obese, you are at increased risk of developing gall stones. Therefore following a low fat diet and increasing your exercise level will not only help you lose weight but also reduce your risk of developing gall stones. However, rapid weight loss can cause the formation of gall stones in some people, so it is important to lose weighgradually.
Gall bladder surgery
Surgical removal of the gall bladder is the most effective means of curing gall bladder disease - the effects are immediate. Once the gall bladder has been removed, however, there is no reservoir of bile, and fat absorption may be affected, in this case, following a low fat diet be helpful.
Coping with Crohn's disease and ulcerative colitis
People who have an inflammatory bowel disorder, such as Crohn's disease or ulcerative colitis, cannot absorb nutrients properly and so are at risk of nutrients deficiencies and becoming underweight.
Getting enough nutrients
If you have an inflammatory bowel disorder, make sure you get enough nutrients. A dietitian can help you in dealing with deficiencies, which can develop because the damaged intestine is not absorbing nutrients effectively. This is very important for children, who are growing and developing. Symptoms such as nausea, diarrhoea, and recurrent abdominal pain can occur at mealtimes, which often leads to decreased appetite and food intake. In Crohn's disease, inflammation of the intestine can result in overgrowth of bacteria. This, combined with the effects of any previous surgery to remove diseased sections of the bowel can decrease the absorptive surface area of the intestine and reduce the absorption of essential nutrients. People who have undergone surgery may have problems absorbing fats and this, coupled with frequent bouts of diarrhoea, may also cause deficiencies to develop.
It is crucial to increase the amount of protein you eat as inflammatory bowel disorders can cause excessive intestinal secretion of protein rich fluids through the inflamed wall of the intestine. Good sources include lean meat, poultry, oily fish and pulses.
Protective foods
Various foods can help relieve as well as prevent the troublesome symptoms of an inflammatory bowel disorder.
- Complex carbohydrates from whole grains, vegetables, and fruits are good source of fibre, which helps the intestine function properly. If the extra fibre causes wind, you can take an over the counter product to reduce this.
- Eat plenty of foods containing omega-3 fatty acids, such as linseed's, rapeseed oil, soya beans, and oily fish.
- Drink lots of fluids, mainly water, but avoid caffeinated drinks. Green tea is thought to be beneficial.
- The herb sage may be helpful too.
Foods to avoid
Certain foods may cause symptoms. Common things to avoid are: alcohol, sugar foods, including sweet fruit such as grapes, and pineapple, and caffeine, as the can all cause inflammation; foods containing gluten, which is found in wheat, oats, and barley; milk and dairy products; foods that are common causes of allergic reactions, such as soya, eggs, and peanuts; and vegetables of the brassica family, such as Brussels sprouts, cabbages, and broccoli.
Taking supplements
People who have Crohn's disease or ulcerative colitis are advised to take a multivitamin supplement. Deficiancies of the fat soluble vitamins (A, D, E, K), vitamin B12, and folate are common. A folate supplement is vital for anyone taking sulfasalazine (a drug prescription for chronic inflammation), which can interfere with folate's absorption. Some patients may need injections of vitamin B12. Persistent, watery diarrhoea may require supplementation with the minerals zinc and magnesium.
Diverticular disorders
Diverticulosis is the presence of small pouches (known as diverticuli) in the wall of the colon, which occur when parts of the intestine bulge outwards through weak areas. The increase in pressure in the colon is commonly caused by constipation due to lack of fibre in the diet. From time to time, one or more of these "pouches" may become inflamed. This condition is known as diverticulitis, and it is possible to treat it with a low fibre, "soft" diet.
High fibre for diverticulosis
Diverticulosis is very common among older people and, although it often does not produce specific symptoms, some people may develop cramps, bloating, and irregular bowel movements, with no sign of fever or infection. Treating and preventing diverticulosis through nutrition often involves just increasing insoluble fibre in the diet, this helps keep stools soft and easy to pass and prevents constipation, and therefore prevents the development of diverticulosis. Experts recommend an intake of at least 18g of fibre from food every day. Fruits, vegetables, and whole grains are good sources od dietary fibre, and can easily be incorporated into your daily diet.
If you suffer from diverticulosis, it is important that you follow a high fibre diet, and make sure that you also drink plenty of fluids (preferably water) about 2 litres a day. It is important that you avoid becoming constipated as hard stools or straining when you go to the toilet will cause more diverticuli (pouches) to form and make your symptoms worse.
Eating seeds and nuts
In the past, doctors recommended that people with diverticulosis should avoid eating nuts and seeds because they could lodge in the diverticula and lead to diverticulitis. There are no known cases of such a blockage. however, and so there is no proven benefit in avoiding seeds and nuts. If you have suffered rectal bleeding, your doctor may still advice you not be eat seeds and nuts, but otherwise you can safely enjoy these foods as part of a high fibre diet.
Low fibre for diverticulitis
Diverticulitis is an acute infection or inflammation of the diverticuli that may flare up if stool gets caught in one of the "puches". Symptoms can include abdominal pain, fever, and nausea. An infection usually lasts for about a week. When someone with diverticulosis develops diverticulitis, the nutritional advice changes. Rather than following a high fibre diet, you should instead follow a low fibre one, which allows the passage of stools through the inflamed, typically narrowed segment of the colon.
In additional, you should eat a soft diet, which means that you should eat things that do not require much chewing, such as soup, mashed potatoes, well cooked pasta, and bananas. Once the infection has cleared up, patients should go bach to their high fibre diet.
Dealing with lactose intolerance
Normally, the enzyme lactase breacks down lactose (a natural sugar found in milk and other dairy products) in the intestine to form the sugars glucose and galactose. These are then easlity absorbed through the intestinal wall into the bloodstream. If this enzyme is absent or its levels are low, the unabsorbed lactose ferments, producing painful symptoms such as abdominal bloating and cramping., diarrhoea, and vomiting. The condition usually develops in adolescence or adithood and is uncommon in babies and young children. No tratment can improve the body's ability to produce lactase, but symptoms can be easily controlled through diet.
Read food labels
If you are lactose intolerant, check food labels very carefully for hidden dairy products. There may be small amounts of lactose in breads, cereals, biscuits, margarine, sliced cooked meats, salad dressings, soups, sweets, and many other foods. Lactose free forms of milk are commonly available.
Limit or avoid lactose
Some people can benefit from just reducing the amount of foods they eat containing lactose, such as milk, yogurt, cheese, cream, and butter, and most are able to tolerate a small amount of lactose withous symptoms. However, some people will develop symptoms from just a tiny amount of lactose. For those who cannot tolerate even small amount of lactose, lactase enxymes are avalable, which will help them digest foods that contain lactose.
Soya alternatives
Try soya milk if you cannot tolerate even lactose free milk. Soya milk is naturally lactose free, yet it supplies many of the same nutrients that are in cow's milk. Different brands of soya milk have different tastes, so try a few until you find one that you like.
Watch your calcium intake
Dairy products are our prime source of dietary calcium, which is important for maintaining bone health. You should therefore try to include some lactose free dairy or soya products in your diet every day. Other calcium tich foods are canned salmon, spinach, and leafy greens. If you fall short on calcium, a supplement of 800-1200mg per day is advisable to maintain the recommended daily calcium levels.
Gluten-free diet for coeliac disease
In coeliac disease, the intestine cannot absorb food property due to a reaction to gluten, a protein found in wheat, rye, barley, and oats. The only treatment, therefore, is a gluten free diet, which must be followed for life. A gluten free diet will improve symptoms within days of starting it, allow existing damage to heal, and prevent further intestinal damage. The table below is a great starting point for anyone embarking on a gluten free diet. Remember always to check food labels for hidden gluten as it can appear in different forms in places you wouldn't expect to find it, for example in hydrolyzed vegetable protein (HVP).
| FOOD TYPE | FOODS ALLOWED | FOODS NOT ALLOWED |
|
Bread, pasta, cereal, rice, and grains |
Bread or pasta made from corn (maize), rice, soya, potato starch, potato flour, whole bean flour, tapioca, sago, rice bran, sorghum, and quinota, cereal containing rice or corn; corn tacos and tortillas |
Breads containing wheat, rye, barley, oats, bran, semolina, kamut; pasta made from wheat or wheat strach; couscous; cereals made from wheat, rye, triticale, barley, oats
|
|
Fruits and vegetables |
Fresh, frozen, and canned fruits and vegetables (avoid emulsifiers and stabilizers from unknown sources) |
Fruit per filling, breadcrumbed or creamed vegetables (read labels)
|
|
Dairy foods |
Milk, cream, buttermilk, yogurt, cheese, cream cheese, processed cheese, and cottage cheese |
Thickened milkshake (some contain flouer); processed cheese products
|
|
Protein foods |
Fresh meat, fish, and poultry; pulses; nuts and seeds; tofu |
Cooked meats, sausages, and canned ham or tuna may contain HVP (check labels)
|
| Fats and oils | Butter, margarine, and vegetable oils | Shredded suet; sprays with grain alcohol |
| Alcohol | Whine, potato, vodka, rum, tequila, and sake |
Beers and ales, grain alcohol, most liqueurs
|
| Miscellaneous |
Home made soups; wheat free soy sauce; non- grain vinegars such as wine or fruit vinegar |
Canned soup; stock cubes, most soya sauces; white vinegar made from grains |
![]()
Disclaimer: This website is for information purposes only. By providing the information contained herein we are not diagnosing, treating, curing, mitigating, or preventing any type of disease or medical condition. Before beginning any type of natural, integrative or conventional treatment regime, it is advisible to seek the advice of a licensed healthcare professional.



























